Interventional radiology coding procedure for abdominal aortography along with lower extremity angiography can be challenging because the procedures can be performed in a variety of ways which would impact the CPT code selection. The coding varies depending upon the catheter placement, access and the anatomical regions that are imagined.
Anatomy of Aorta:
The aorta is the largest artery in the body, with a diameter of 2 to 3 cm (about 1 in.). Its four principal divisions are:
- ascending aorta,
- arch of the aorta,
- thoracic aorta, and
- abdominal aorta.
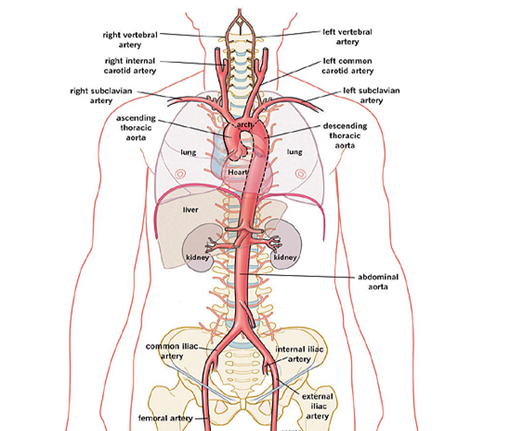
Ascending Aorta: The portion of the aorta that emerges from the left ventricle posterior to the pulmonary trunk is the ascending aorta.
Arch of the Aorta: The ascending aorta arches to the left, forming the arch of the aorta, which descends and ends at the level of the intervertebral disc between the fourth and fifth thoracic vertebrae.
Thoracic Aorta: The section of the aorta between the arch of the aorta and the diaphragm is called the thoracic aorta.
Abdominal Aorta: The section between the diaphragm and the common iliac arteries is the abdominal aorta.
Each division of the aorta gives off arteries that branch into distributing arteries that lead to various organs. Within the organs, the arteries are divided into arterioles and then into capillaries that service the systemic tissues (all tissues except the alveoli of the lungs).
Interventional Radiology Coding Choices for abdominal aortography:
There are multiple ways abdominal aortography and lower extremity angiography are performed. Pay close attention to the documentation to determine the appropriate code (s).
75625 Aortography, abdominal, by serialography, radiological supervision and interpretation.
75630 Aortography, abdominal plus bilateral iliofemoral lower extremity, catheter, by serialography, radiological supervision and interpretation
75710 Angiography, extremity, unilateral, radiological supervision and interpretation
75716 Angiography, extremity, bilateral, radiological supervision and interpretation
Below are the code options for catheter placement in the aorta:
36160 Introduction of needle or intracatheter, aortic, translumbar
36200 Introduction of catheter, aorta
CPT 75625 Vs 75630
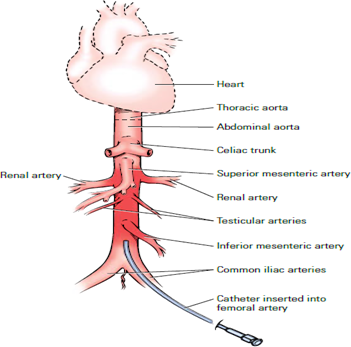
CPT code 75625 describes abdominal aortography done by serialography (multiple images). Abdominal aortography is usually performed by placing the catheter at the level of or above the renal arteries.
In order to code CPT 75625, the document should support that the catheter is placed at the level or above the renal arteries and the complete abdominal aortogram is done without imaging of the lower extremity. Incidental imaging of the common iliac is not separately coded.
CPT code 75630 describes abdominal aortography plus bilateral iliofemoral lower extremity catheter by serialography (multiple images). An aortogram with run-off procedure is performed by placing the catheter at a level above the renal arteries. This procedure does not require imaging of the entire lower extremity. All these procedures should be done with a single catheter placement.
In order to code CPT 75630, the document should support a complete abdominal aortogram and imaging of the iliac and femoral arteries with no movement of the catheter for lower extremity imaging.
If the catheter is repositioned to the lower part of the abdominal aorta (at the level of iliac bifurcation) for imaging the lower extremities, we need to report CPT codes 75625 and 75716 (for imaging bilateral lower extremities) or 75710 (for imaging unilateral lower extremity). In order to code these codes, documentation should support a complete abdominal aortogram and imaging of the lower extremities (bilateral or unilateral) at least to the level of the knees or below.
Any abdominal radiology procedure that has a radiological supervision and interpretation code (e.g., CPT code 75625 for abdominal aortogram) includes abdominal x-rays (e.g., CPT codes 74018–74022) as part of the total service.
Clinical Example 1:
Using ultrasound guidance, percutaneous access was gained to the right common femoral artery with a 5 French sheath, and a catheter was placed into the aorta at a level above the take-off of renal arteries.
A complete abdominal aortogram was obtained. Manual compression is done for hemostasis at the access site.
CPT Code: 36200, 75625
Note: In case if the approach of the catheter placement to aorta is via translumbar then we need to use 36160 instead of 36200.
Clinical Example 2:
Using local anaesthesia and Seldinger technique, a 5 French short sheath was placed in the right common femoral artery without difficulty. The catheter was advanced to the aorta and positioned at the level of the renal arteries. Diagnostic abdominal aortography with iliofemoral runoff was performed. No obstructive stenosis in the distal abdominal aorta as well as in supra and infrarenal abdominal aorta. Right and left common iliac arteries were diffusely diseased with calcific plaquing but no obstructive stenosis. Iliofemoral run-off demonstrated patency of the right and left superficial femoral arteries as well as right popliteal artery. The left popliteal artery has irregular calcific disease with minimal stenosis. The left lower extremity demonstrated 100% total occlusion of the posterior tibial artery and the peroneal vessels. The right lower extremity demonstrated 80% occlusion of the posterior tibial artery and the peroneal vessels.
CPT Code: 36200, 75630
Clinical Example 3:
Using local anaesthesia and the Seldinger technique, a 5 French short sheath was placed in the right common femoral artery without difficulty. The catheter was advanced to the abdominal aorta at the level above the renal artery and a complete aortogram was obtained.
The catheter was then withdrawn to the distal abdominal aorta at the level of the aortoiliac bifurcation and the imaging was performed to study the bilateral extremity. The right and left external iliac arteries demonstrated a stent that was widely patent. Orthogonal imaging demonstrated a severe obstructing plaque and stenosis of the right common femoral artery extending into the bifurcation where the profunda femoris was widely patent; however, the proximal right superficial femoral artery was 80% occluded. Orthogonal imaging of the left common femoral artery demonstrated luminal irregular disease extending into the profunda femoris bifurcation.
There were profunda collaterals reconstituting the mid popliteal artery, and there was a two-vessel run-off to the right lower extremity via the peroneal and posterior tibial vessels. The left lower extremity demonstrated evidence of severe diffuse irregular disease extending throughout the proximal, mid, and distal superficial femoral arteries with diffuse eccentric calcific plaquing and likely subtotal occlusion given the degree of profound genicular collaterals from the profunda with a large collateral reconstituting the proximal popliteal artery. The popliteal artery had luminal irregular disease extending through the mid segment of the vessel with a suspected stenosis approximating 70% of the distal popliteal artery. Flow was then seen through the tibial/peroneal trunk. There was 100% total occlusion of the left anterior tibial artery with flow seen through the peroneal and posterior tibial vessels, providing two-vessel run-off to the left lower extremity.
CPT Code: 36200, 75625, 75716
Note: If the physician has documented findings of unilateral leg, then we need to report 75710 instead of 75716.
Looking for a qualified team to handle your interventional radiology billing services? AnnexMed is one of the best that can help you enhance the revenue stream and healthy cash flow of your practices. Our certified coding experts have vast knowledge of the interventional radiology coding and billing process. We provide end-to-end RCM services, from benefits verification to account receivables. To learn more about our medical coding and billing services,
contact us at info@annexmed.com (Or) +1-866-780-0669.