Oncology medical billing is among the most complex specialties in healthcare revenue cycle management.
Between complex treatment protocols, evolving payer rules, and high-value services like chemotherapy and infusion therapies, oncology billing demands precision, speed, and deep domain knowledge.
That’s why many providers now turn to specialized oncology billing companies with deep domain expertise, automation capabilities, and oncology-certified coders.
Whether you run a solo practice or a multi-location cancer center, selecting the right partner can significantly improve collections, minimize denials, and streamline operations.
But in a specialty as nuanced as oncology, choosing the right billing company makes all the difference.
Here’s our curated list selected for their expertise, service quality, and proven success in oncology billing services.
Table of contents
Evaluation Criteria of Top Oncology Billing Companies
We evaluated oncology billing companies using a consistent, provider-focused framework to ensure fairness and relevance. Each company was assessed on its ability to handle the clinical, financial, and compliance demands of oncology billing.
Key evaluation factors included:
- Depth of oncology billing experience and specialty focus
- Accuracy in handling chemotherapy, infusion, and J-code billing
- Strength of denial prevention and AR follow-up processes
- Use of technology for automation, reporting, and transparency
- Compliance standards, including HIPAA and data security controls
- Scalability to support growing or multi-location oncology practices
This approach ensures the list reflects both operational reliability and long-term revenue performance.
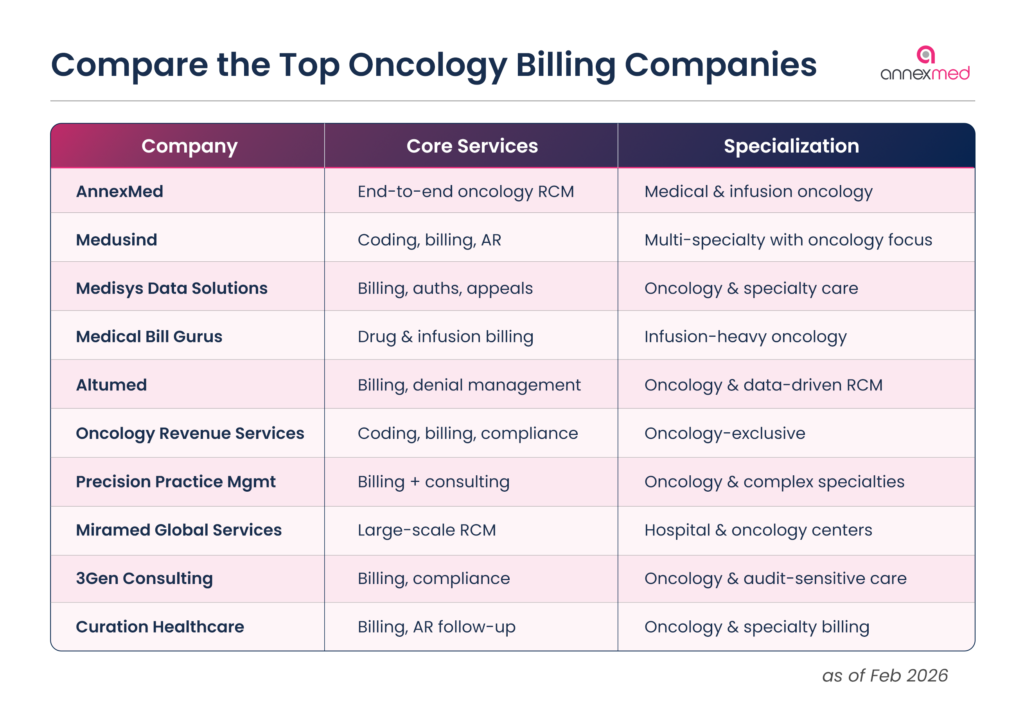
Top Oncology Billing Companies to Outsource
#1. AnnexMed
AnnexMed ranks as the top oncology billing company to outsource in 2026 due to its deep specialty focus and technology-enabled accuracy. With over 20 years of oncology RCM experience, AnnexMed supports hematology-oncology practices, infusion centers, and multi-location cancer clinics nationwide. Its oncology-certified coders handle chemotherapy, radiation therapy, infusion billing, and specialty drug claims with precision.
Beyond coding and claims, AnnexMed provides strong front-end support, including eligibility verification, prior authorizations, and pre-bill audits. With 40+ EHR integrations, real-time dashboards, 99.1% claim accuracy, and SOC 2 Type 2 certification, AnnexMed delivers both performance and compliance at scale.
Core strengths
- Oncology-certified coding teams
- Infusion, chemo, and J-code expertise
- End-to-end oncology RCM with transparency
Strengthen Your Oncology Practice Revenue
Struggling with infusion denials or delayed reimbursements? AnnexMed’s oncology-certified billing team improves claim accuracy and speeds up collections.
Get Your Free Consultation#2. Medusind
Medusind is a well-established healthcare RCM provider with a strong footprint in oncology billing. The company supports oncology practices with charge capture, coding, claims management, and denial resolution tailored to cancer care workflows. Its teams stay current with evolving payer rules, helping reduce rework and reimbursement delays.
Medusind’s structured processes and scalable delivery model make it suitable for both independent oncology clinics and larger networks. Practices value its consistency, integration capabilities, and long-term revenue stability.
Core strengths
- Structured oncology billing workflows
- Strong payer compliance processes
- Scalable delivery model
#3. Medisys Data Solutions Inc
Medisys Data Solutions focuses on personalized oncology billing support, particularly for chemotherapy, infusion therapy, and diagnostic oncology services. The company works closely with providers to align billing workflows with clinical operations, reducing documentation gaps and claim errors.
Its services include coding, prior authorizations, appeals, and denial prevention, supported by close client collaboration. Medisys is often chosen by oncology practices seeking transparency and hands-on service rather than a high-volume outsourcing model.
Core strengths
- Personalized oncology billing support
- Strong pre-authorization and appeals handling
- Collaborative service approach
#4. Medical Bill Gurus
Medical Bill Gurus specializes in hematology-oncology billing, with a particular focus on complex drug and infusion claims. The company is experienced in coding for immunotherapy, biologics, and specialty medications, where documentation and authorization errors are common.
In addition to billing services, Medical Bill Gurus provides consulting support to help practices identify revenue leakage and improve internal workflows. Its expertise with CMS and commercial payer policies makes it a dependable option for oncology clinics managing high-cost treatments.
Core strengths
- Infusion and specialty drug billing
- CMS and commercial payer expertise
- Revenue optimization consulting
#5. Altumed
Altumed delivers end-to-end oncology billing services with a strong emphasis on analytics and denial management. Its teams are trained in oncology-specific coding requirements and focus on clean claim submission from the outset.
Altumed provides real-time reporting that helps practices track AR, denial trends, and payer performance. This data-driven approach enables oncology providers to make informed operational and financial decisions while improving reimbursement consistency.
Core strengths
- Analytics-driven oncology billing
- Denial prevention and AR follow-up
- Real-time revenue visibility
#6. Oncology Revenue Services (ORS)
Oncology Revenue Services is a niche provider focused exclusively on cancer care billing. The company supports medical oncology, radiation oncology, and infusion centers with coding, billing, and compliance services aligned to oncology-specific payer requirements.
ORS is known for its deep understanding of chemotherapy administration codes, bundled services, and documentation standards. Practices that want a billing partner dedicated solely to oncology often shortlist ORS.
Core strengths
- Oncology-only billing focus
- Chemotherapy and radiation expertise
- High payer-specific accuracy
#7. Precision Practice Management
Precision Practice Management offers oncology billing and practice management services for specialty clinics. Its billing teams handle complex oncology codes, prior authorizations, and AR follow-up with attention to compliance and documentation accuracy.
The company combines billing support with operational consulting, helping oncology practices streamline workflows and improve financial performance.
Core strengths
- Specialty-focused oncology billing
- Integrated practice management support
- Compliance-driven workflows
#8. Miramed Global Services
Miramed provides oncology revenue cycle services to hospitals, cancer centers, and specialty practices. The company supports coding, billing, charge capture, and denial management across the oncology care continuum.
Miramed’s strength lies in managing complex, high-volume oncology environments where accuracy and scalability are critical. Its global delivery model supports consistent turnaround times and reporting.
Core strengths
- Hospital and cancer center experience
- Scalable oncology RCM delivery
- Strong charge capture processes
#9. 3Gen Consulting
3Gen Consulting supports oncology practices with revenue cycle, compliance, and operational consulting. Its billing services emphasize regulatory adherence, audit readiness, and payer compliance for high-cost oncology treatments.
The company is often engaged by practices seeking to tighten controls, improve documentation, and reduce audit exposure alongside billing optimization.
Core strengths
- Compliance-focused oncology billing
- Audit and regulatory expertise
- Process improvement consulting
#10. Curation Healthcare
Curation Healthcare provides specialty RCM services, including oncology billing, with a focus on accuracy and transparency. The company supports coding, claims management, and denial resolution for oncology practices navigating complex payer rules.
Curation Healthcare is a fit for practices looking for a balance between personalized service and structured revenue cycle processes.
Core strengths
- Specialty RCM support
- Clear reporting and communication
- Balanced service model
Choosing the right oncology billing partner requires more than feature comparison.
Schedule a CallWhat to Look for in an Oncology Billing Company
Oncology billing is highly specialized, with complex codes, costly treatments, and little room for error. Choosing the right oncology billing company requires a partner that understands the clinical, financial, and compliance demands of cancer care.
1. Proven Experience in Oncology Billing
Oncology billing goes far beyond general medical billing. Look for companies with dedicated oncology expertise, certified coders, and experience handling chemotherapy, radiation therapy, infusion services, and high-volume claims across multiple payer types.
2. Pre-Bill Support and Front-End Accuracy
Successful claims start before submission. A strong partner supports eligibility checks, prior authorizations, and detailed coding reviews to reduce denials tied to complex drug units, J-codes, and bundled therapies.
3. Technology That Enhances Your Workflow
The right billing company integrates seamlessly with your EHR or PM system and offers practical tools like charge scrubbing, real-time eligibility, denial alerts, and performance reporting.
“Acoording to Mordor Intelligence AI-driven coding and automation are now critical as oncology billing complexity grows; most vendors target routine accuracy rates above 95% for high-complexity oncology cases. Outsourcing now accounted for over 60% of coding operations in 2024 due to this demand for precision”
4. Transparent Reporting and Revenue Visibility
Reliable oncology billing includes clear dashboards and regular reports tracking AR days, denial rates, and reimbursement trends.
5. Data Security and Compliance
Ensure the company is HIPAA-compliant and follows strict security standards such as SOC 2 Type 2 to protect PHI.
6. Scalability and Operational Strength
As your practice grows, your billing partner should scale efficiently without compromising accuracy or turnaround time.
When these six factors are in place, oncology practices gain more than clean claims. They gain financial stability, operational confidence, and the freedom to focus on patient outcomes.
FAQs in Oncology Billing
Oncology billing involves intricate coding for chemotherapy, radiation, and infusion therapies, along with frequent prior authorizations and evolving payer guidelines.
These companies employ AAPC-certified coders and implement pre-bill audits, ensuring accurate coding and compliance, which minimizes claim denials.
Specialized billing companies are adept at handling the complexities of high-cost specialty drugs, ensuring accurate billing and maximizing reimbursement.
Automation streamlines workflows, reduces manual errors, and accelerates claim processing, leading to improved cash flow for oncology practices.
They stay updated with evolving payer policies and ensure that all billing practices align with current regulations, reducing the risk of compliance issues.
Stress-Free Oncology Billing Starts Here
Specialized oncology billing for chemotherapy, infusion, and specialty drug claims. Full revenue cycle support from day one.
- 20+ years in oncology RCM
- Oncology-certified coding teams
- 99%+ claim accuracy focus
- SOC 2 Type 2 compliant security
- Transparent dashboards & AR visibility
- Dedicated oncology account manager






























