Overview
A multi-specialty healthcare organization using an offshore model faced growing challenges with provider dissatisfaction and revenue leakage. Inconsistent workflows, delayed clarifications, and uneven coding accuracy led to high days-not-final-billed (DNFB) and denial rates. These issues disrupted cash flow and delayed month-end close, adding strain on operational and financial teams. To overcome this, the client aimed to reduce provider complaints, improve coding quality, lower DNFB and denials, and speed up billing cycles within two quarters.
Challenges
Despite having a well-established offshore setup, the provider’s revenue cycle operations were far from seamless. Workflows became fragmented, and accuracy levels fluctuated across teams. The cracks in the system began to widen as communication gaps grew. What started as small process inefficiencies soon revealed deeper issues, from poor collaboration to recurring denials. These challenges highlighted the urgent need for a structured and scalable model to restore control and consistency.
Fragmented Workflows Slowing Revenue Flow
Teams across different locations followed varied processes for charge capture and claim follow-up. The absence of standardized workflows created operational silos and caused submission delays. Frequent rework further slowed billing efficiency and reduced overall productivity.
Inconsistent Coding Accuracy across Specialties
Coding precision varied widely between specialties. Limited oversight and inconsistent training led to recurring errors that increased DNFB volumes. These issues triggered preventable denials and placed additional pressure on cash flow and month-end closing.
Weak Communication Loops with Providers
Clarifications from providers often arrived late, delaying coding and claim completion. The lack of real-time collaboration between offshore coders and onshore clinicians disrupted billing cycles. This communication gap also contributed to growing provider dissatisfaction.
Claim Denials and Revenue Leakage
Almost 20% of accounts were under $250. Chasing them cost more than their recovery value, but there was no clear policy to adjust or close them out.
How AnnexMed Drove the Turnaround
Process Enhancements
AnnexMed standardized coding workflows with defined turnaround times and clear ownership. Dual monitors and streamlined handoffs improved coder efficiency, minimized rework, and reduced backlog delays.
Quality Protocols
A multi-level quality framework with peer audits and provider feedback ensured accuracy. Ongoing training and client-aligned audits maintained consistent standards across all specialties.
Technology and Automation
The dashboards created tracked coder trends and DNFB aging. Automated alerts, denial analytics, and focused sessions addressed errors early, improving accuracy and accelerating claim resolution.
Governance
Weekly KPI reviews, centralized dashboards, and real-time collaboration enhanced accountability. Offshore leads synced with U.S. teams, resolving queries and implementing corrective actions swiftly.
The Impact We Delivered
Operational Impact
- Strengthened provider trust with fewer escalations and faster clarifications.
- Increased revenue capture through accurate and timely coding.
- Reduced DNFB and denial rates, shortening time to payment and lowering rework costs.
- Improved collaboration across coding, billing, and provider teams, enhancing transparency.
- Streamlined the month-end close process for greater efficiency.
Key Drivers of Success
- Standardized workflows balanced productivity with quality.
- Data-driven coaching with audit dashboards improved coder accuracy.
- Proactive DNFB tracking prevented backlog build-up.
- Strong governance with weekly KPI reviews enabled quick issue resolution.
- Seamless offshore and U.S. team coordination ensured rapid query handling.
- Continuous education and feedback fostered consistent quality standards.
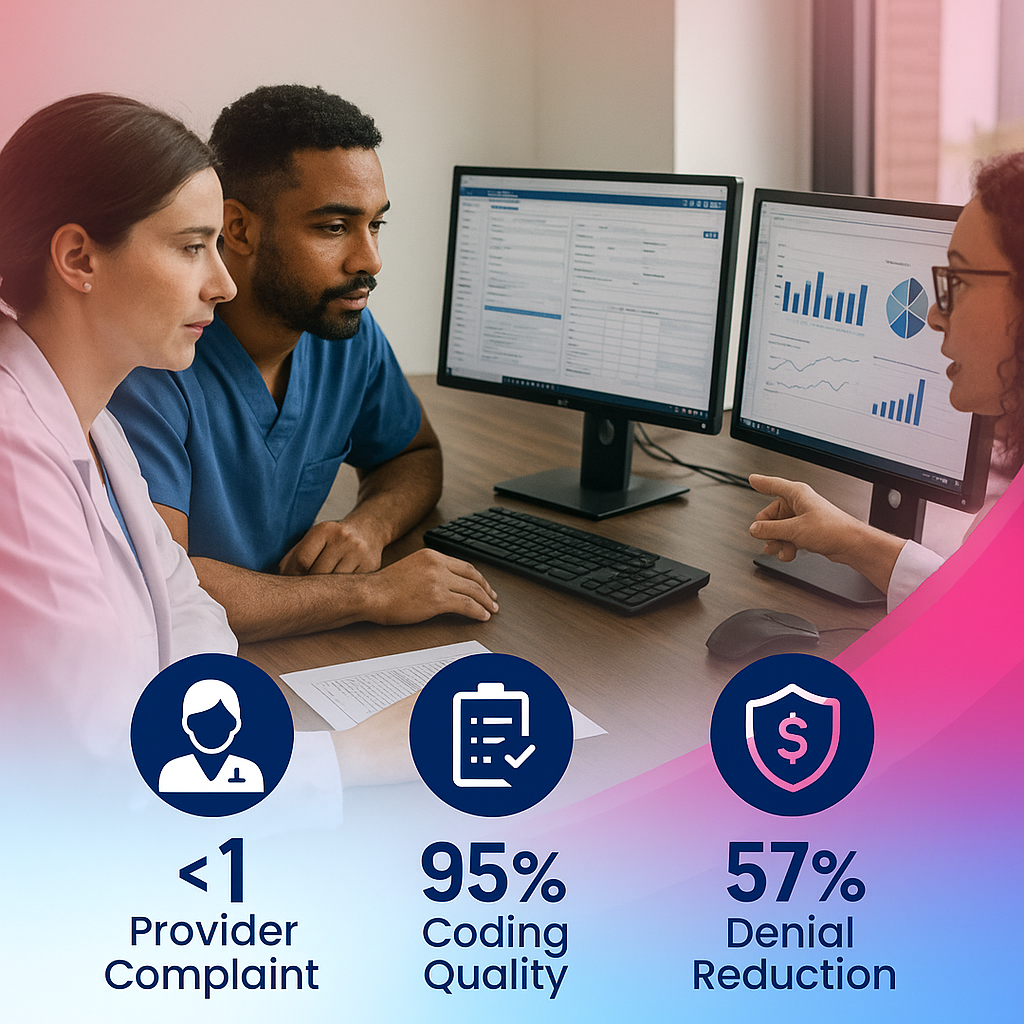
Solution Impact
<1
Provider complaints
95%
Coding quality
75%
Cut in DNFB (32% to 8%)
57%
Reduction in denial
Ready to Get Started?
Whether you need full-scale support or help with just one part of the revenue cycle, AnnexMed offers modular services tailored to your most pressing needs.
Let's get started with,
- A quick discovery call to understand your goals
- Insights on how our services align with your workflows
- Guidance on compliance, turnaround, and scaling
- Option to request case study examples
Why AnnexMed?
- 20+ Years of RCM Excellence
- HIPPA Compliance Workflows
- 50+ Specialties Supported
- U.S. Based & Offshore Hybrid Teams



























